If you have been diagnosed with an enlarged prostate due to BPH, there are several treatment options available. Consult your physician to determine which treatment is right for you.
Treatment Options
Watchful Waiting
When symp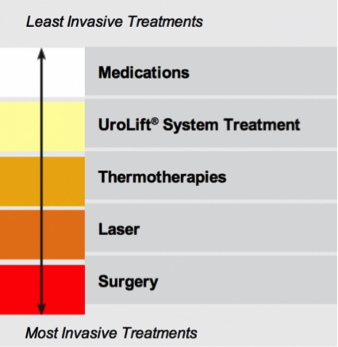 toms are mild, your doctor may just monitor your condition and ask you to track your symptoms before deciding if any treatment is necessary.
toms are mild, your doctor may just monitor your condition and ask you to track your symptoms before deciding if any treatment is necessary.
Medications
Your doctor may prescribe medications to manage your symptoms. These medications include alpha blockers which relax the muscles around the neck of your bladder, making it easier to urinate, and alpha reductase inhibitors which act to shrink the prostate. While medications can be helpful in relieving symptoms for some men, patients must continue taking them long-term to maintain the effects.
Some patients may suffer side-effects including dizziness, headaches, or sexual dysfunction. Some may not get adequate relief of their symptoms. Over 16% of men on medication for BPH discontinue treatment early for reasons such as being dissatisfied with side-effects or not getting adequate symptom relief.
UroLift® System Treatment
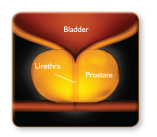
The UroLift® System treatment is a minimally invasive approach to treating BPH that lifts or holds the enlarged prostate tissue out of the way so it no longer blocks the urethra. There is no cutting, heating or removal of prostate tissue. Clinical data has shown that the UroLift System treatment is safe and effective in relieving lower urinary tract symptoms due to BPH without any impact to sexual function.



Learn more about how the UroLift System treatment works or visit our FAQ page for more information on the benefits, risks, and recovery.
Rezūm
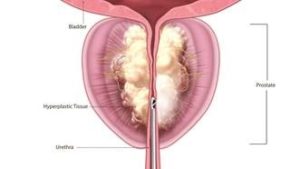
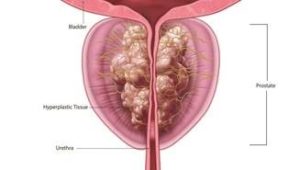
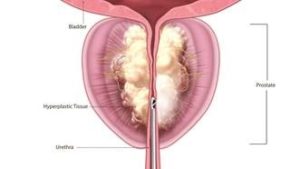
Rezūm is a treatment for BPH that can be performed in a clinic or out-patient setting. Rezūm uses the stored thermal energy in water vapor (steam) to treat the extra prostate tissue that is causing symptoms such as frequency, urgency, irregular flow, weak stream, straining and getting up at night to urinate.
Inside a hand-held device, radiofrequency energy is applied to a few drops of water to create vapor (steam). The water vapor is injected into the prostate tissue that is blocking the flow of urine from the bladder, where it immediately turns back to water, releasing the energy stored in the vapor into the cell membranes. At this point, the cells are gently and immediately damaged, causing cell death. Over time, your body will absorb the treated tissue through its natural healing response.
Rezūm provides the following benefits:
- Potential alternative to BPH medications
- Relieves symptoms safely and effectively1
- Provides noticeable symptom improvement within two weeks
- Simple in-office/out-patient therapy
- Does not require general anesthesia
- Preserves sexual and urinary functions1
- Allows patients to return to regular activities within a few days1
We are the 1st clinic in Georgia approved to perform this cutting-edge procedure.
1 McVary KT et al. Minimally Invasive Prostate Convective Water Vapor Energy (WAVE) Ablation: A Multicenter, Randomized, Controlled Study for treatment of Lower Urinary Tract Symptoms Secondary to Bening Prostatic Hyperplasia. J Urol. 2015 Nov 22. pii: S0022-5347(15)05258-1. doi: 10.1016/j.juro.2015.10.181. [Epub ahead of print] – update to new citation
Learn more about Rezūm Water Vapor Therapy at http://www.rezum.com/the-rezum-system/.
Thermotherapies
Thermotherapies are minimally invasive treatments where heat energy such as microwave or radiofrequency is applied to destroy prostate tissue. Less invasive than TURP, these treatments are generally safe, can be performed under local anesthesia and provide moderate symptom relief for some patients.
Applying high heat to the prostate can cause tissue swelling and uncomfortable urinary symptoms during the healing period. Symptom relief does not occur immediately, and patients often need to have a catheter that is attached to a urine bag inserted into their bladder during the recovery period.
Laser
Laser Resection of the Prostate
TURP may be performed with a laser in procedures called photoselective vaporization of the prostate (PVP) or holmium laser enucleation (HOLEP). Laser therapy lessens the bleeding risks of traditional TURP. However, since prostate tissue is still removed, there can be tissue swelling and an uncomfortable healing time. Typically, a catheter has to be inserted into the bladder after the procedure.
Surgery
Transurethral Resection of the Prostate (TURP)
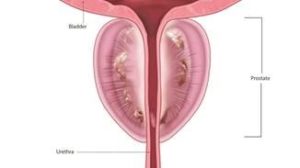
TURP is the most common surgery to treat BPH. During this procedure, patients undergo general anesthesia, and prostate tissue is removed. TURP is often considered the “gold standard” for long-term results.
After prostate tissue has been removed, the body needs time to heal. The remaining prostate tissue may actually swell and become inflamed before the desired shrinking effect occurs. Patients may suffer an uncomfortable recovery period that includes short-term problems such as bleeding, infection, erectile dysfunction, and urinary incontinence. Patients have to
have a catheter that is attached to a urine bag inserted into their bladder for several days after the procedure.
Symptom relief may not occur immediately, but lasts for a long time in many patients once it does occur.
There can be long-term side effects after TURP such as dry orgasm (retrograde ejaculation), erectile dysfunction or incontinence (leaking of urine).








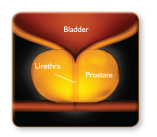
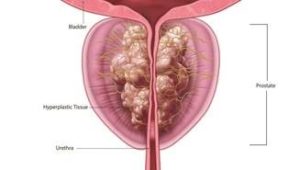
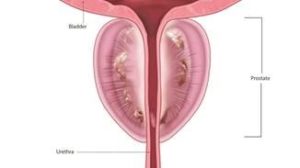
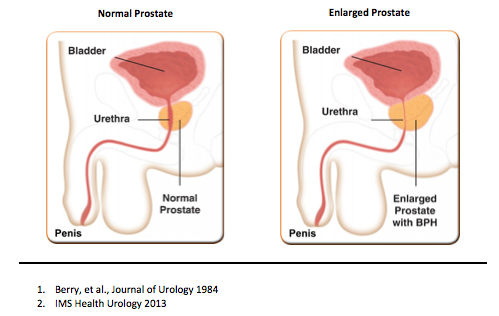 Benign Prostatic Hyperplasia, or BPH, is a condition in which the prostate enlarges as men get older. Over 70% of men in their 60s have BPH symptoms so it is very common1. While BPH is a benign condition and unrelated to prostate cancer, it can greatly affect a man’s quality of life.
Benign Prostatic Hyperplasia, or BPH, is a condition in which the prostate enlarges as men get older. Over 70% of men in their 60s have BPH symptoms so it is very common1. While BPH is a benign condition and unrelated to prostate cancer, it can greatly affect a man’s quality of life.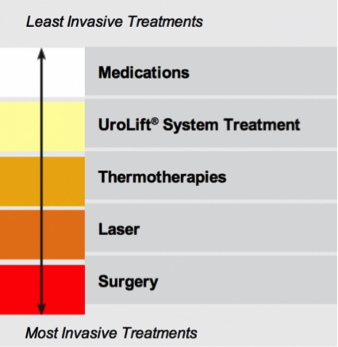 toms are mild, your doctor may just monitor your condition and ask you to track your symptoms before deciding if any treatment is necessary.
toms are mild, your doctor may just monitor your condition and ask you to track your symptoms before deciding if any treatment is necessary.