Laboratory testing begins with a semen analysis. To perform this, a man is asked to produce a semen sample through masturbation, either at home or in a private area of the office, and return the sample to the laboratory within one hour (prompt return is essential). It is important to collect all the ejaculated fluid. The man should not ejaculate for 48 to 72 hours before the semen collection.
The sample will be analyzed to determine:
- Amount of ejaculate
- Number of sperm
- Percent motility and progression – how well sperm are able to swim and move forward
- Morphology – the percentage of sperm that have a normal shape
- Sperm agglutination – whether the sperm clump together abnormally
- Semen viscosity – whether the semen liquifies and flows properly
- Pyospermia – the presence of white blood cells, which may indicate infection
Table 1. Semen Analysis: Minimal Standards of Adequacy
On at least two occasions:
| Ejaculate volume: | 1.5–5.0 cc |
| Sperm density: | >20 million/cc |
| Motility: | >60% |
| Forward progression: | >2 (scale 1–4) |
| Morphology: | >60% normal |
And:
No significant sperm agglutination
No significant pyospermia
No hyper viscosity
Because these results can vary from one semen sample to another, every patient should have this test repeated at least once.
Testing Semen Hormone Levels
A routine part of the initial male evaluation is measuring the level of hormones in the serum (blood), including FSH, LH, testosterone, prolactin, and estradiol. The way these 5 hormones interact is closely tied to normal sperm production. Abnormalities may signal a problem in the hypothalamus, pituitary gland, or testicle.
Semen Leukocyte Testing
Increased numbers of leukocytes (white blood cells) in the semen have been associated with problems with sperm function and motility and may be due to infections or inflammation. Special staining techniques have been developed to detect white blood cells in the semen. If high levels are detected, the doctor should perform a semen culture — another type of lab test to spot infection.
White blood cells in the semen are also associated with the release of harmful substances called reactive oxygen species (ROS), which will be discussed in more detail below.
Antisperm Antibody (ASA) Testing
Antisperm antibodies (ASAs) are immunoglobulins created by a man’s own immune system that attack his normal, healthy sperm. These antibodies can cause the sperm to clump together and reduce their motility.
The presence of ASAs in the semen may signal genital or urinary infections, trauma to the testes, thermal injury, or an obstruction in the genital tract.
Reactive Oxygen Species (ROS)
Reactive oxygen species, or oxidants, are highly reactive chemicals containing oxygen that can injure the sperm and the genital tract and impair sperm function. Specialized semen testing can determine whether ROS levels are too high.
Morphology Testing
Analyzing the morphology (shape) of the sperm can offer clues about how they develop and function.
There are two methods for evaluating sperm morphology. Standard tests using a standard microscope provide a crude estimate of the percentage of sperm with normal shape. A more specialized test, known as “strict morphology,” which provides more detail, can only be conducted by trained technicians in specialized male fertility labs.
DNA Damage
DNA can be examined under a microscope to determine whether certain strands are broken or damaged. Damaged DNA can create abnormal embryos which fail to grow properly and are lost through miscarriage. Two main causes of DNA damage are cigarette smoking and the exposure to toxins in the environment.








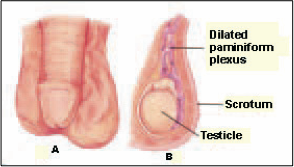 Varicocele Repair
Varicocele Repair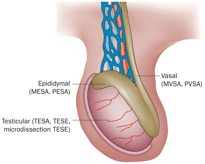 epididymal sperm aspiration (MESA) is a technique for the procurement of sperm from the epididymis of men in whom transport of sperm from the testicle to the ejaculate is not possible because the drainage (ductal) system is absent or is not subject to reconstruction. This problem most commonly occurs in men with vasal agenesis, a condition in whic
epididymal sperm aspiration (MESA) is a technique for the procurement of sperm from the epididymis of men in whom transport of sperm from the testicle to the ejaculate is not possible because the drainage (ductal) system is absent or is not subject to reconstruction. This problem most commonly occurs in men with vasal agenesis, a condition in whic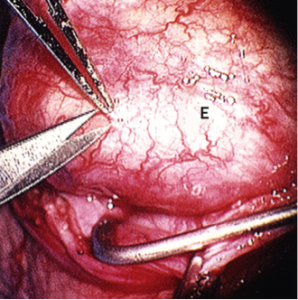 on is not possible or not desired by the couple, MESA is carried out. During MESA, sperm are directly aspirated from a single, isolated epididymal tubule until 10–20 million are obtained. The entire procedure is performed through an operating microscope. When the aspiration is completed, the epididymal tubule is closed with multiple microscopic sutures and the scrotum is closed in a routine surgical fashion. The recovery period is approximately 24 hours. Sperm, which have been aspirated, are specially processed and prepared for insemination with the wife’s eggs. The procedure is routinely performed in advance of the IVF with intracytoplasmic sperm injection (ICSI) cycle so that the couple can be assured adequate sperm are extracted and available on the day of oocyte retrieval. Recent data indicate that there are no differences between fertilization and pregnancy rates when frozen rather than fresh sperm are utilized.
on is not possible or not desired by the couple, MESA is carried out. During MESA, sperm are directly aspirated from a single, isolated epididymal tubule until 10–20 million are obtained. The entire procedure is performed through an operating microscope. When the aspiration is completed, the epididymal tubule is closed with multiple microscopic sutures and the scrotum is closed in a routine surgical fashion. The recovery period is approximately 24 hours. Sperm, which have been aspirated, are specially processed and prepared for insemination with the wife’s eggs. The procedure is routinely performed in advance of the IVF with intracytoplasmic sperm injection (ICSI) cycle so that the couple can be assured adequate sperm are extracted and available on the day of oocyte retrieval. Recent data indicate that there are no differences between fertilization and pregnancy rates when frozen rather than fresh sperm are utilized.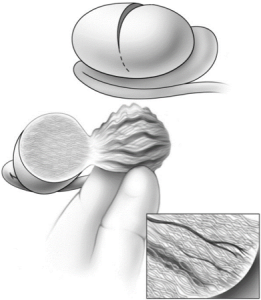 put is mapping out the location of sperm in the testicle. It is a procedure performed for men who have both a sperm production problem and are azoospermic. A surgeon will perform this in the operating room with general anesthesia under the operating microscope. Micro-TESE is carefully coordinated with the female partner’s egg retrieval, and is typically performed the day before egg retrieval. This
put is mapping out the location of sperm in the testicle. It is a procedure performed for men who have both a sperm production problem and are azoospermic. A surgeon will perform this in the operating room with general anesthesia under the operating microscope. Micro-TESE is carefully coordinated with the female partner’s egg retrieval, and is typically performed the day before egg retrieval. This